Pay Commission
OPSC ASO Admit Card 2025 Out at opsc.gov.in, Exam on 9th November
Salary & Allowance
OPSC ASO Admit Card 2025 Out at opsc.gov.in, Exam on 9th November
Retirement
OPSC ASO Admit Card 2025 Out at opsc.gov.in, Exam on 9th November
Govt Schemes & Opportunities
OPSC ASO Admit Card 2025 Out at opsc.gov.in, Exam on 9th November
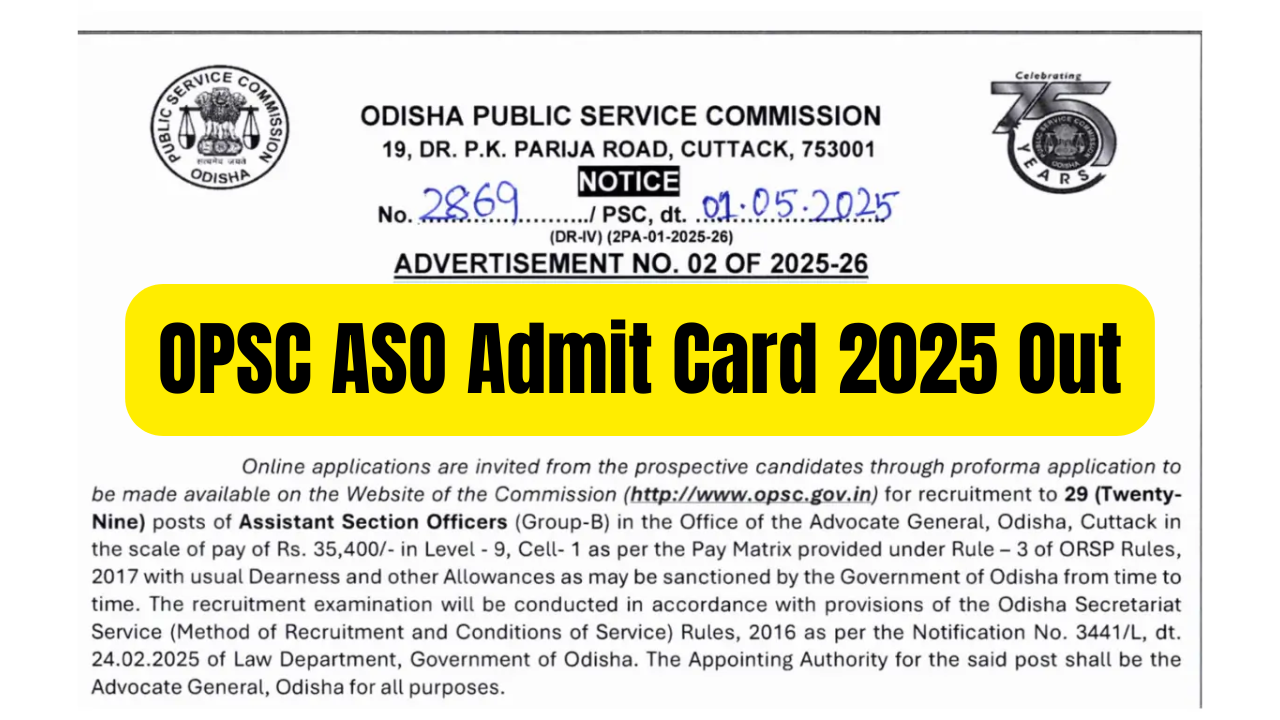
The Odisha Public Service Commission (OPSC) has officially released the OPSC ASO Admit Card 2025 on its website — https://www.opsc.gov.in/….